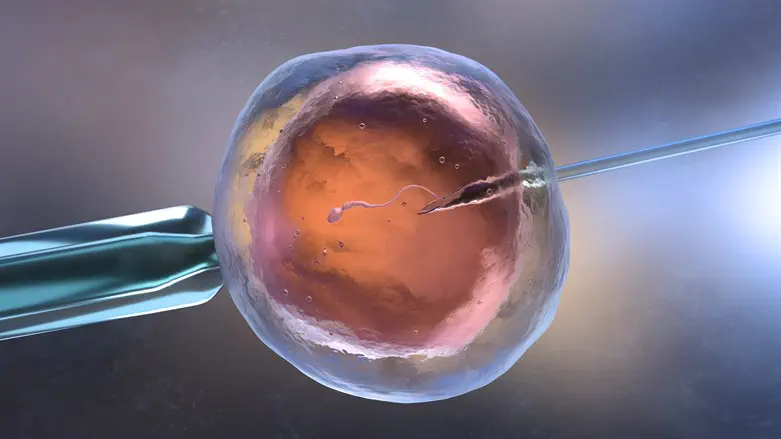
Israel's Health Ministry has released new guidelines for sperm donation, addressing the recent changes in the industry and aiming to balance demand with the protection of both donor rights and the health of the resultant offspring
The new guidelines, now open for public comments, represent an improvement in the treatment standard in the field, and include a requirement for donors to undergo comprehensive genetic testing, as well as limits on the number of families who can receive donations from a single donor.
Recent years have seen several trends in sperm donation: an increase in demand, particularly among single women and same-sex couples, while the number of Israeli donors has not risen and does not meet demand; an increase in the cost of foreign sperm donations; and difficulty recruiting donors due to stricter requirements, with only about 15% of interested applicants qualifying, alongside a significant rise in prices due to the need for numerous tests.
Two-and-a-half years ago, the Ministry of Health established a Fertility and Birth Department to regulate fertility treatments in Israel. As part of this, changes were made to procedures and Ministry directives, and oversight in the field was enhanced. Currently, 17 sperm banks operate in Israel under the Ministry Director-General’s circular from 2007. In light of the many changes in the field, the Ministry has decided to update the circular and relevant procedures.
The updated Health Ministry guidelines present rules for the management and licensing of sperm banks, regulating the operation of sperm bank laboratories, guidelines and limitations on accepting sperm from Israeli donors, genetic and other testing for donors, the reception of foreign sperm donations, importation mechanisms, allocation of sperm donations to recipients, sperm retrieval from banks, medical record management, and provisions for self-use sperm deposits, the preservation of minors' sperm, the retrieval of sperm from deceased individuals, and safety, confidentiality, and data security protocols.
The directive also includes clear guidelines for medical and genetic testing for donors and minimum medical conditions for receiving a donation, including obtaining full medical history, conducting comprehensive genetic testing, and storing DNA for future tests, both from domestic and international donors.
Among the key regulations is the management of sperm donor registries by the Ministry, in a move intended to prevent a donor from donating at more than one sperm bank. The database also aims to allow secure transmission of information between banks regarding genetic findings and other findings discovered in offspring, to reduce the risk of genetic diseases in future offspring.
Sperm donations from a single donor are limited to up to 12 families, and additionally, up to five women requesting fertility preservation only.
Given the responsibility of sperm bank managers in matching donors to recipients, the procedure mandates that recipients undergo at least the genetic tests included in the "health basket" to reduce the risk of genetic diseases to a minimum, as much as possible.
Further, the procedure requires reporting to the manager of the relevant sperm bank and the Ministry of Health regarding any genetic or potentially genetic findings in offspring from sperm donations, to assess whether to continue using the donation and prevent harm to future offspring. It also defines the minimum information to be provided to recipients about the donor, including their declared religion and any additional halakhic (pertaining to Jewish law) information provided.
Additionally, a sperm donor will be able to indicate on the consent form that if, in the future, non-anonymous sperm donation becomes legally possible, they would be interested in considering it, subject to the law and the legal situation at that time. The guidelines continue to require the recipient’s consent, and that of their spouse or partner if applicable, for the use of donated sperm, with the agreement that the children born from it will be considered their legal children for all purposes, including child support and inheritance. At the same time, the guidelines also recommend that couples prepare a will.
To increase the pool of donors, men up to the age of 38 will be allowed to donate sperm. It was also established that a married or cohabiting donor may donate sperm, but must declare that they have informed their wife or partner.
In June, The Israeli Ministry of Health announced that following the death of a sperm donor, it was discovered that he carried a genetic mutation associated with Lynch syndrome - an inherited condition that significantly increases the risk of certain cancers, particularly of the colon and uterus.
The Ministry recommends that individuals born from sperm donations conducted in central Israel between 1974 and 1985, as well as women who received these donations, undergo genetic testing at an appropriate laboratory. The identified mutation is MSH2 1906G→C, which carries a 50% hereditary risk.
This test is not currently included in the "basket" of subsidized medical tests, and those seeking testing are advised to contact their health funds for further evaluation or genetic counseling.
